Neuropathic pain is a complex condition caused by nerve damage or dysfunction, often leading to chronic, debilitating discomfort. As healthcare providers, understanding its unique characteristics is key to effective diagnosis and management. This guide covers its mechanisms, symptoms, and evidence-based treatment strategies to improve patient outcomes.
What is Neuropathic Pain?
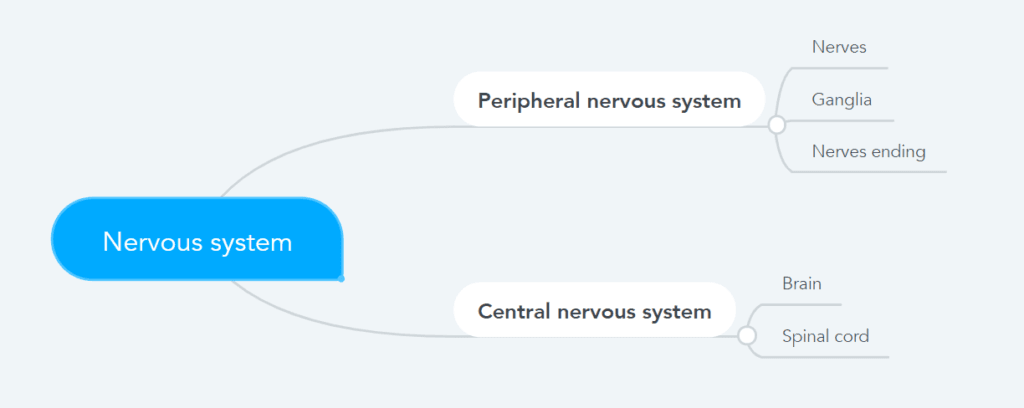
Neuropathic pain results from abnormal nerve signaling, differing from nociceptive pain, which comes from tissue damage. In neuropathic pain, the nerves misfire, creating pain where there’s no external injury.
Key Characteristics:
- Chronic: Persistent pain requiring long-term care.
- Hyperexcitability: Nerves are oversensitive, amplifying pain signals.
- Spontaneous pain: Occurs without an obvious trigger.
Clinical Presentation: Symptoms and Red Flags
Symptoms vary but often include:
- Burning sensations: Described as deep, persistent heat.
- Shooting or electric-like pain: Sharp jolts radiating along nerve pathways.
- Paresthesia: Tingling or "pins and needles."
- Allodynia: Pain from normally non-painful stimuli.
- Hyperalgesia: Exaggerated pain responses.
These signs help distinguish neuropathic pain from other types and guide diagnosis.
Causes and Risk Factors
Common causes of neuropathic pain include:
- Diabetic Neuropathy: Often presenting as distal symmetric polyneuropathy.
- Postherpetic Neuralgia: Persistent pain after shingles.
- Trauma: Injuries, surgeries, or repetitive strain affecting nerves.
- CNS Disorders: Conditions like multiple sclerosis or stroke.
- Cancer Treatments: Chemotherapy-induced peripheral neuropathy (CIPN).
Neuropathic pain requires an individualized, multidisciplinary approach. By combining medications, physiotherapy, and lifestyle changes, practitioners can improve patient outcomes. Collaboration among healthcare teams is key, as is staying up to date with the latest practices to provide the best care.


No Comments